Estimated reading time: 14 minutes
Author’s Note:
This article was initially published in 2014. Since then, a growing body of research has strengthened the case for using the triglyceride-to-HDL cholesterol (TG/HDL-C) ratio as a simple, powerful marker of cardiometabolic risk. This 2025 update brings new clinical insight, clearer explanations, and a narrative approach to help readers understand why this ratio matters more than ever.
For decades, cholesterol has been the headline act in our understanding of heart disease. High LDL-cholesterol (LDL-C) — the so-called “bad” cholesterol — was cast as the main villain, while HDL-cholesterol (HDL-C) earned praise as the “good” kind. Statins became the blockbuster therapy, and LDL-C targets the cornerstone of prevention guidelines.
But heart disease is more nuanced than a single number.
LDL-C tells us something — but not everything. Many patients with metabolic dysfunction carry substantial cardiovascular risk, even when their cholesterol levels appear “normal.” Their danger lies not just in how much cholesterol they carry, but in how it’s packaged.
Case in Point: John’s Heart Attack Wasn’t Predicted by LDL-C
Marvin was 52, tied to a desk, with a widening waistline. His LDL-C was 116 mg/dL (3.0 mmol/L) — “normal,” according to his doctor. But he had a strong family history of heart disease, borderline blood pressure, and signs of metabolic stress.
His labs showed triglycerides at 210 mg/dL (2.4 mmol/L), HDL-C at 38 mg/dL (1.0 mmol/L) — a TG/HDL-C ratio of 5.5. That ratio is a red flag for insulin resistance and an atherogenic lipid profile, often overlooked when LDL-C is the sole focus.
No further steps were taken.
Six months later, John had a heart attack. A ruptured plaque in his LAD artery triggered a clot that blocked blood flow to a large part of his heart.
The warning was there, just not recognized.
A high TG/HDL-C ratio is a strong marker of insulin resistance and an atherogenic lipoprotein profile, meaning it reflects a pattern that promotes plaque formation in the arteries. Yet it’s often ignored in favor of LDL-C alone.
Despite mounting evidence, the triglyceride-to-HDL cholesterol (TG/HDL-C) ratio remains underrecognized in clinical practice. Multiple studies have found the TG/HDL-C ratio to be a stronger predictor of cardiovascular risk than LDL-C alone, particularly in individuals with metabolic syndrome, obesity, or type 2 diabetes.
This article examines why the TG/HDL-C ratio warrants greater clinical attention: what it reveals about lipoprotein behavior, what the science says, and how it fits into a more accurate, metabolically informed approach to cardiovascular risk assessment.
Understanding Lipoproteins: The Real Players
When people say, “My cholesterol is normal,” they usually mean their LDL-C — the amount of cholesterol inside LDL particles — looks okay on their lab report. But that number doesn’t always tell the whole story.
Here’s why.
Cholesterol can’t float freely in the blood. It’s a fat, and fat doesn’t mix with water. So the body packages it into tiny particles called lipoproteins — protein-coated carriers that transport not just cholesterol, but also triglycerides and phospholipids, to and from cells.
You can think of them as delivery trucks in your bloodstream.
There are different kinds:
- Chylomicrons carry fat from food after you eat.
- VLDL (very-low-density lipoproteins) deliver triglycerides made in the liver.
- LDL (low-density lipoproteins) carry mostly cholesterol.
- HDL (high-density lipoproteins) help remove excess cholesterol from the bloodstream.
- Lp(a) [Lipoprotein(a)] is a genetically determined LDL-like particle linked to increased cardiovascular risk.
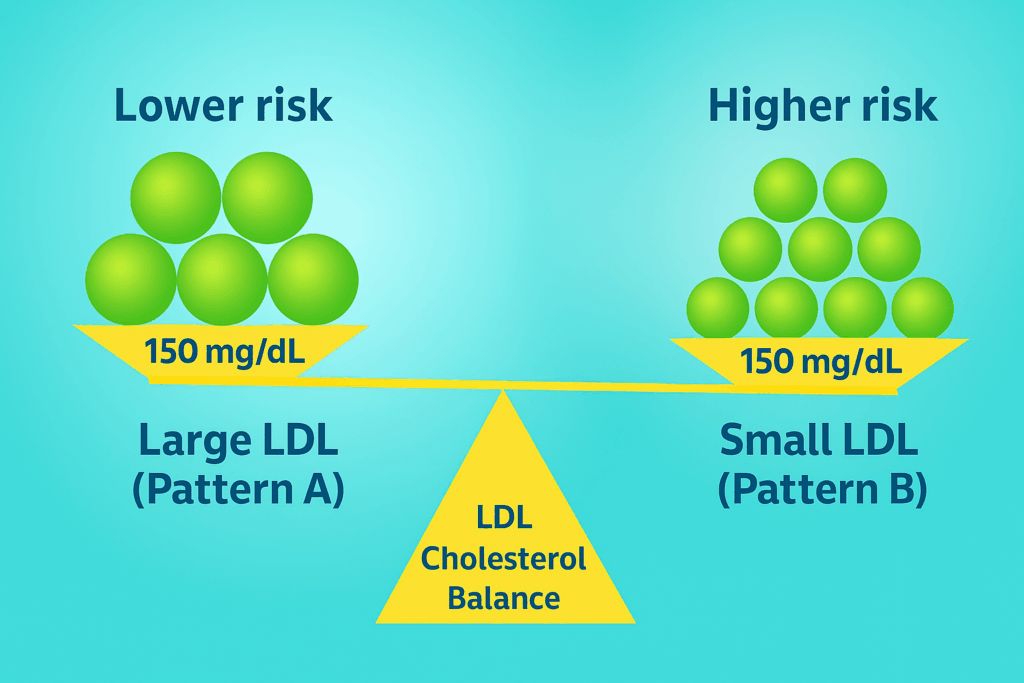
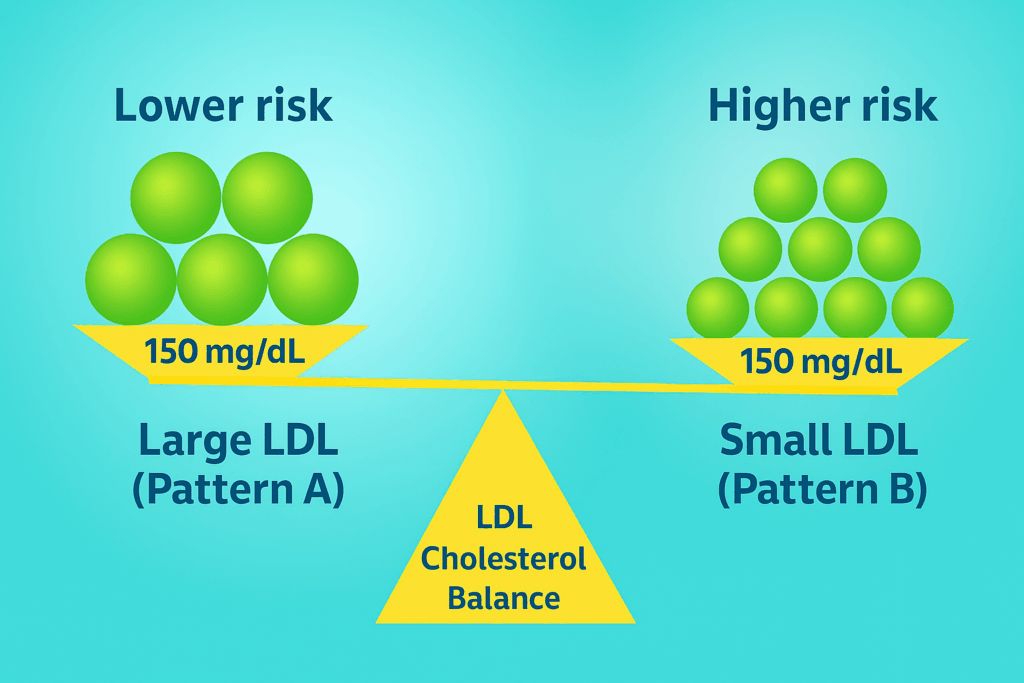
Now here’s the key insight: some of these trucks are more dangerous than others, especially small, dense LDL particles. They can more easily penetrate the arterial wall, become oxidized, and trigger inflammation. Over time, this contributes to the buildup of plaque and the development of atherosclerosis.
The LDL-C Problem
LDL-C tells you how much cholesterol is inside LDL particles — but it doesn’t tell you how many particles are present. That’s a problem, because a patient may have low LDL-C but still carry a high number of small, dense LDL particles — each only lightly loaded with cholesterol, but still atherogenic.
This mismatch, when particle number is high but cholesterol content appears “normal,” is called lipid discordance. Studies consistently show that cardiovascular risk tracks more closely with the number of particles than with the total cholesterol they carry.
LDL-P and ApoB: Two Ways to Count the Trucks
So, how do we measure the number of atherogenic lipoproteins?
There are two validated ways:
-
LDL-P (LDL particle number), measured via nuclear magnetic resonance (NMR)
-
Apolipoprotein B (ApoB), a protein carried on every atherogenic particle, including VLDL, IDL, LDL, and Lp(a)
Every one of these particles carries exactly one molecule of ApoB. So while LDL-P gives you a particle count from one subclass (LDL), ApoB gives you the total count of all atherogenic particles.
The two markers correlate closely, and both are stronger predictors of cardiovascular risk than LDL-C.
The next step is to understand what the TG/HDL-C ratio can tell us, and why it’s so practical.
The Lipid Panel: What We Measure and What We Miss
The standard lipid panel has been a cornerstone of cardiovascular risk assessment for decades. It measures:
- Total cholesterol
- LDL cholesterol (LDL-C)
- HDL cholesterol (HDL-C)
- Triglycerides (TG)
Importantly, LDL-C is not measured directly in most cases — it’s typically calculated using the Friedewald formula, which estimates LDL-C based on total cholesterol, HDL-C, and triglycerides. This approach is most effective when triglyceride levels are within the normal range and the patient is fasting; however, its reliability decreases at high triglyceride levels or in individuals with metabolic disturbances.
LDL-C has historically received the most attention — and with good reason. Numerous studies have linked elevated LDL-C with increased risk of heart disease, and LDL-lowering therapies like statins have proven benefits.
The LDL-C problem becomes especially important in people with metabolic syndrome, insulin resistance, or type 2 diabetes. These individuals often have a seemingly normal LDL-C, yet elevated cardiovascular risk. Why? Because they tend to have high levels of triglyceride-rich lipoproteins (like VLDL), low HDL, and a high number of small, dense LDL particles.
The standard panel misses this pattern — unless you know where to look.
The Clue in the Ratio
The TG/HDL-C ratio offers a simple but powerful clue. It reflects underlying lipid dynamics that the LDL-C number can’t capture, particularly in people with metabolic dysfunction.
A high TG/HDL-C ratio is often a sign of:
- Increased VLDL secretion
- Reduced HDL-mediated reverse cholesterol transport
- Smaller, denser LDL particles
- Higher likelihood of elevated ApoB and LDL particle number
In other words, the ratio can unmask atherogenic dyslipidemia — a common but often overlooked driver of cardiovascular disease.
Why Use TG/HDL-C Instead of ApoB or LDL-P
While ApoB and LDL particle number (LDL-P) provide more direct measurements of atherogenic burden, they require advanced testing that is not available everywhere and often comes with additional costs.
In contrast, the TG/HDL-C ratio is calculated from the standard lipid panel, which is routinely ordered in clinical practice. It costs nothing extra, requires no special lab equipment, and still offers valuable insight into lipoprotein size, particle number, and metabolic health.
It’s not a perfect substitute, but it’s a practical, powerful tool hiding in plain sight.
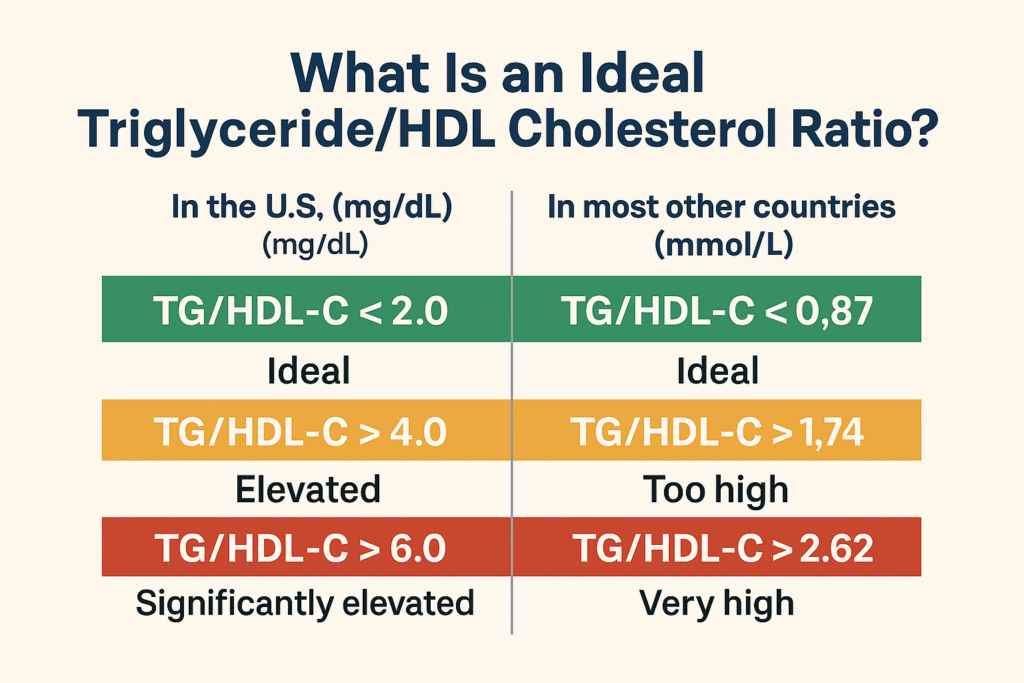
What Is an Ideal TG/HDL-C Ratio?
The triglyceride-to-HDL cholesterol ratio is easy to calculate:
Just divide your fasting triglycerides by your HDL cholesterol — using the same units.
However, there is one crucial detail: different countries report lipids in different units.
In the U.S. (mg/dL):
-
TG/HDL-C → Ideal
-
TG/HDL-C > 4.0 → Elevated
-
TG/HDL-C > 6.0 → Significantly elevated, suggests atherogenic dyslipidemia
In most other countries (mmol/L):
To convert mg/dL to mmol/L, multiply your ratio by 0.4366.
Or, if you’re going the other way (mmol/L → mg/dL), multiply by 2.3.
📌 Note: In this article, we use the U.S. convention (mg/dL) unless otherwise specified.
What the TG/HDL-C Ratio Tells Us About LDL Particles
One of the most fascinating — and clinically useful — insights about the TG/HDL-C ratio is its ability to reveal the type of LDL particles in circulation.
As we’ve seen, not all LDL particles are created equal. Some are large and buoyant, others small and dense. And that difference matters.
Why Particle Size Matters
Small, dense LDL particles are more atherogenic. They’re:
People with insulin resistance, abdominal obesity, or metabolic syndrome often have a predominance of these small, dense LDL particles — even when their LDL-C is “normal.”
The Ratio Predicts Particle Size
Several studies have shown that the TG/HDL-C ratio correlates with LDL particle size. One found that:
-
Among people with a TG/HDL-C ratio above 3.8, about 80% had a predominance of small, dense LDL
-
Among those with a ratio below 3.8, about 80% mainly had large, buoyant LDL
This makes sense biochemically.
When triglycerides are elevated — often due to excess VLDL — an exchange occurs: triglycerides move from VLDL into LDL and HDL, while cholesteryl ester moves in the opposite direction. This transformation leaves LDL and HDL particles enriched in triglycerides and depleted in cholesterol.
Then, when lipases remove those excess triglycerides, the particles shrink, leaving behind smaller, denser LDL.
Particle Number Still Matters More
Size alone isn’t the whole story. While small LDL particles are more dangerous on a per-particle basis, the number of LDL particles (LDL-P) — or their surrogate, ApoB — is often a stronger predictor of cardiovascular risk.
Fortunately, a high TG/HDL-C ratio usually reflects both small particle size and high particle number, especially in the context of metabolic disease.
So while the TG/HDL-C ratio doesn’t directly measure ApoB or LDL-P, it points us in the same direction, often with remarkable accuracy.
TG/HDL-C Ratio and Insulin Resistance
Discover more from Doc’s Opinion
Subscribe to get the latest posts sent to your email.